Abstract
Introduction Low blood oxygen (hypoxia/hypoxemia) is common in people living with sickle cell disease (SCD), and has been attributed to combinations of hypoventilation, diffusion impairment, intracardiac/intrapulmonary shunts, and/or ventilation/perfusion mismatch. Low oxygen has been associated with high reticulocyte counts, abnormal red blood cell rheology, and cerebrovascular disease in homozygous sickle cell anemia (SCA), but its prevalence and impact on disease progression in adults is not well understood. Our primary objective in this study was to assess the prevalence of low oxygen in a cohort of adults living with SCD, focusing on occult night-time hypoxemia (nocturnal hemoglobin desaturation (NHD)). Our secondary objective was to explore the association between NHD and clinical history and lab values.
Methods In this single institution cross-sectional study, we assessed NHD in adults with SCD genotype HbSS and HbSβ0-thlassemia, with a history of priapism, nocturnal symptoms, and/or an absolute reticulocyte count (ARC) above 275 x 103 cells/μL. Oximetry was performed with the WatchPAT™ ONE home sleep apnea test device. The threshold for identification of NHD was a measured SpO2 ≤ 88% for ≥ 5 minutes of sleep time, per Medicare guidelines for eligibility for oxygen therapy. Clinical data via medical chart abstraction and patient reported outcomes (ASCQ-Me Pain Impact, PROMIS Fatigue, and Pittsburgh Sleep Quality Index) were collected prospectively upon enrollment. All participants gave informed consent, and the protocol was reviewed by the University of North Carolina Institutional Review Board.
Results Twenty-four individuals were consented for the study, with 20 completing their oximetry testing. These participants ranged in age from 21 to 46 years (median 38, interquartile range [IQR] 33-43). Nineteen participants had HbSS, and one had HbSβ0-thalassemia. Nine participants (45%) were positive for NHD and were prescribed oxygen, with a median time at or under 88% SpO2 (desaturation time) of 31.6 minutes (IQR 19.7-226.4). Three participants had extreme desaturation times, >200 minutes, while all others were <75, and these 3 were excluded from analyses of clinical associations.
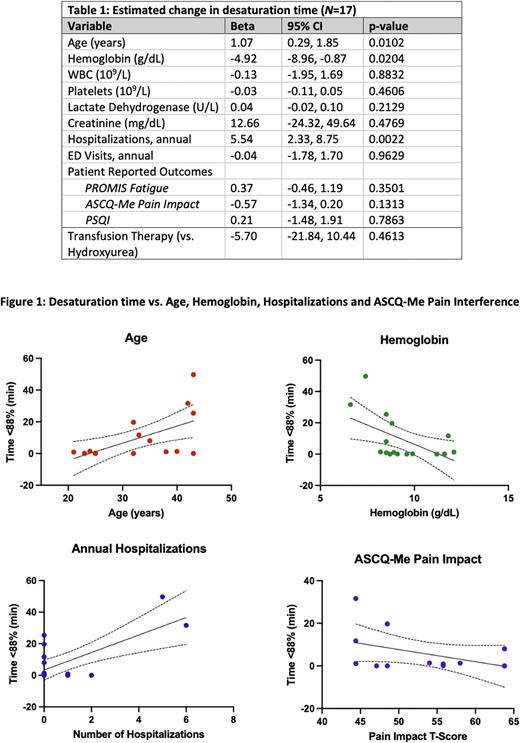
Of the 17 evaluable participants, we found that increasing age, more hospitalizations, and decreased hemoglobin associated with more hemoglobin desaturation at night (Table 1 & Figure 1). Conversely, hemolysis (e.g. LDH and ARC) did not associate with the extent of hemoglobin desaturation; however, ARC was not a reliable indicator because of its central role in selection criteria. Reported pain impact, fatigue, and worsening sleep quality were not unequivocally associated with NHD in this small sample.
Conclusion In a selected subset of people living with SCA, 45% had NHD of sufficient degree to be eligible for oxygen therapy per Medicare guidelines. Longer NHD times associated with anemia, increased age, and more hospitalizations. In ongoing work, we are examining the impact of oxygen therapy, qualitatively and quantitatively, on clinical measures and red blood cell health in this population, seeking to learn whether screening for occult hypoxemia could improve clinical outcomes in people living with SCA. Limitations of this study include the small sample size and strict selection criteria, constraining its power to represent the SCA population as a whole. Nonetheless, this pilot study suggests that NHD is more common in adults with SCA than is generally appreciated, and may be of clinical relevance.
Disclosures
Little:bluebird: Research Funding; FORMA: Other: Adjudication Committee; GBT: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal